How to Beat Premenstrual Dysphoric Disorder Naturally
Premenstrual Dysphoric Disorder (PMDD) is an extreme form of Premenstrual Syndrome (PMS).
So consider what is typically associated with PMS - mood swings, irritability, bloating, pain, cravings, headaches and generally feeling unwell. With PMDD expand these symptoms into 1, 2 and even 3 weeks prior to menstruation and multiply them in severity by 2 to 10 times... Then you have an understanding of what PMDD is like. It's extreme and it's life-destroying.
The general population have often not even heard of PMDD, and even people close to a sufferer of PMDD struggle to understand the condition. This is, of course, assuming it has actually been diagnosed, which is often not the case.
So it's complicated, it's difficult to treat and the causes are misunderstood in the mainstream medical system. Honestly, it’s a huge problem and women who have PMDD need a lot of support and guidance to overcome this debilitating condition.

Symptoms
| Psychological symptoms: | |
| Irritability | Nervousness |
| Agitation | Anger |
| Difficulty concentrating | Depression |
| Anxiety | Confusion |
| Lack of control | Severe fatigue |
| Insomnia | Forgetfulness |
| Poor self-image | Paranoia |
| Emotional sensitivity | Crying spells |
| Moodiness | Trouble sleeping |
| Fluid Retention: | |
| Swelling of the ankles, hands, and feet | Periodic weight gain |
| Diminished urine output | Breast fullness and pain |
| Respiratory problems: | |
| Allergies | Infections |
| Visual Problems: | |
| Vision Changes | Eye Infections |
| Gastrointestinal symptoms: | |
|
Abdominal cramps
|
Bloating
|
| Constipation |
Nausea
|
| Vomiting |
Pelvic heaviness or pressure
|
| Backache |
| Skin problems: | |
|
Acne
|
Cold sores
|
| Aggravation of other skin disorders | Skin inflammation with itching |
| Neurologic and vascular symptoms: | |
| Headache | Dizziness |
|
Fainting
|
Nausea
|
|
Heart palpitations
|
Easy bruising |
|
Numbness, prickling, tingling, or heightened sensitivity of arms and/or legs
|
Muscle spasms
|
| Other: | |
|
Decreased coordination
|
Painful menstruation
|
| Diminished sex drive | Appetite changes |
| Food cravings | Hot flashes |
PMDD is extreme, and it's diagnosed not through a blood or saliva test, but simply through presentation of symptoms that are severe and last across the cycle.
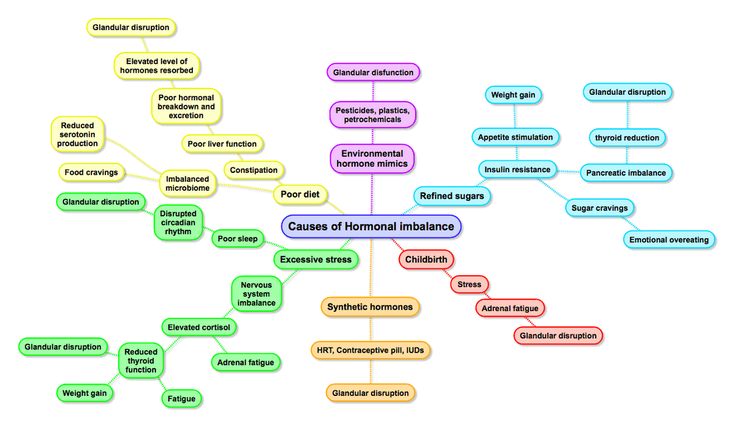
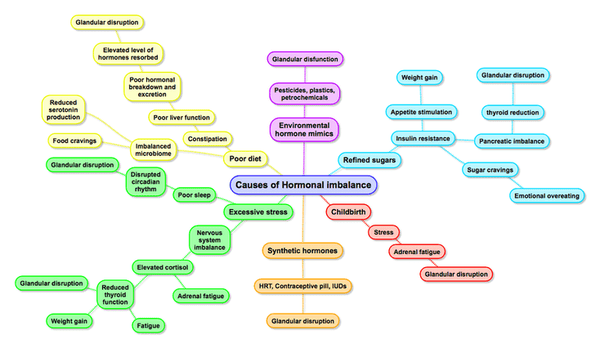
Causes
There is no proven cause of PMDD, and it’s a controversial topic among doctors and sufferers as to what really causes the symptoms of PMS to become so severe and spread across the cycle.
According to my experience treating PMDD clinically, several common threads tend to show.
Firstly, and in all cases of PMDD, I have observed there's a history of hormonal issues from a young age. This indicates that from the beginning of their reproductive cycle these women have difficulties metabolising sex hormones.
The surge in hormone levels during teenage years can be very challenging. The most common form of treatment for these girls is the contraceptive pill, which in most cases makes things worse because of course you already have difficulty metabolising hormones.
A whole range of other treatments, mostly based around hormones, are suggested; until eventually surgery is the only option. In between, a range of anti-depressants will usually be prescribed; and often secondary conditions develop, such as endometriosis and polycystic ovarian syndrome.
Now to dig a little deeper into why these women have difficulty metabolising hormones, it's not just genetics - although it’s a common predisposition.

The bowels' ability to clear oestrogens, in particular, is of key importance. When the bowels are not regular, there is a secondary absorption into the bloodstream. So when additional synthetic hormones are added to the system, the emotional symptoms just get exacerbated.
Healthy bowel function is controlled by the diet and the bacterial balance in the gut. So a diet high in processed foods, with a history of antibiotics, can be predisposing factors towards PMDD.
The other aspect that signals a close relationship with the gut and PMDD is that 90% of the body's serotonin levels are produced in the gut. It is postulated that depression and mood disorders are associated with low serotonin levels, and one of the conventional treatments is SSRI antidepressants.
Secondary to this philosophy is the liver's ability to conjugate (break down) hormones. If the liver is not working well, then hormones are excreted into the bowels. And again - if the bowels are not clearing effectively, then a multiplying effect of the hormones occurs.
The final piece of this puzzle lies in the brain - in the hypothalamus and pituitary axis (HPA) which controls hormone levels. This centre in the brain is affected by poor metabolism of hormones and elevated circulating hormone levels.
This causes the body to reduce its own internal production. A confusion is created in the HPA, and hormone levels shift too frequently and eventually cause the long-term symptoms of PMS that become PMDD.

Other factors that contribute to PMDD is a diet high in sugar, wheat and dairy - which create minor allergic reactions leading to adrenal exhaustion, along with stress levels causing elevated cortisol, which further disrupts the HPA axis.
Treatments
Conventional treatments are largely palliative and aim to manage symptoms. There is no real effective treatment option apart from pain-killers and antidepressants.
Our solution to the issue is to deal with the core HPA imbalance in the brain by attempting to balance the control centre with proven herbal medicines such as Sage, Black Cohosh and Vitex.
Without this intervention rarely do you see improvement in the condition. The key is the combination of these three herbal medicines. Taking them singularly is often not effective.
It's also important to stimulate the liver function via specific amino acids and herbal medicines, such as dandelion, milk thistle, methionine and carnitine. Hormone metabolism is then improved.
Improving digestive regularity assists the excretion of hormones; and the use of fermented drinks and foods helps to rebalance the natural gut ecology, to assist in improving serotonin levels and natural hormone breakdown in the gut.
Finally, a healthy lifestyle must be adhered to during the recovery phase, which can take up to a year.
So a diet high in antioxidant foods, alkaline foods and low in processed foods is critical.
Our 8-Week Program gets women started on the right course to eating well.
Exercise is also very important and our Plyocentric Exercises are excellent to improve blood circulation to the pelvic region and manage the physical symptoms of PMDD.
Premenstrual Dysphoric Disorder is not a life sentence. There are very real treatment options; but it takes a partnership between natural medicines, diet and lifestyle. Only then can real changes occur.